MEDIA RELEASE
AI - Your Secret Weapon against Fraud, Waste, and Abuse
As technology has progressed, fraud, waste, and abuse (FWA) and billing schemes have also evolved in both speed and sophistication. This is because technology makes it easier for bad actors to accelerate abusive billing and referral schemes. In simple terms, bad actors have been winning the billing war by adopting technology faster than healthcare and workers' compensation plans. However, with advanced AI technologies, this tech gap does not have to continue, and winning the FWA war has never been more attainable.
AI Is Your FWA Secret Weapon
How do you need to think about AI in terms of winning the FWA war in your workers’ compensation plan? Here are some key ways AI empowers you:
- See “everything” around the entire episode of care in near real-time.
- Analyze every provider bill, patient encounter, and provider relationship in the context of all historical and current activities.
- Continuously credential providers to ensure they are eligible on every bill.
- Detect provider behaviors, schemes, patterns, outliers, and relationships in near real-time to prevent overpayment and ensure patient safety.
Think Like Your Favorite Investigative Thriller
Shows depicting the NSA or CIA racing against time to save the nation and the world are fascinating. That scenario is similar to what workers’ compensation administrators are facing every day. While under assault from bad actors, your plan is trying to care for workers and save the company.
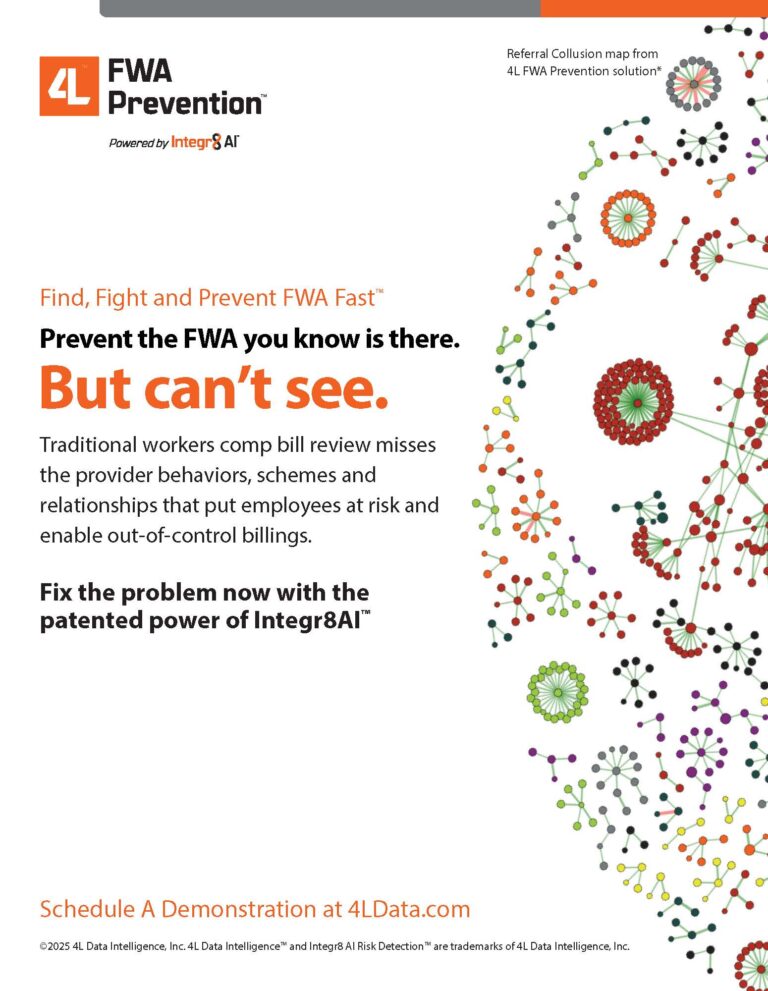
Integr8 AI Risk Detection™ technology is an advanced, patented AI platform that powers the 4L FWA Prevention™ solution. The Integr8 AI patent was issued for the detection of operational threats using artificial intelligence. A second patent was recently issued for collusion detection.
Overbilling and fraudulent referral schemes involving physicians, attorneys, pharmacies, or non-emergency medical transport companies are your daily ‘operational threat’. A technology platform like Integr8 AI enables you to see your FWA and overbilling threats as they are forming, in near real-time and in time to prevent overpayments and ensure the well-being of your employees and members.
AI Turns Simple Bill Review into A Sophisticated Overpayment Detection Machine
Bill review today is usually an old-school, rules-based process. The result is massive overpayment because bills are reviewed individually rather than being analyzed in relationship to all providers and all bills (current and historical).
With advanced AI, you can now understand a bill in the context of how that bill fits into all other bills. It’s like turning the light on in a room versus shining a flashlight into one corner of the room. You need to see “everything” to understand the one thing completely. With a technology like Integr8 AI powering the 4L FWA Prevention™ solution, this means that simple CMS edits turn into over 5.8 million sophisticated permutations and combinations of analyses including procedures and episodes of care on every claim.
AI Saves More & Costs Less Than Traditional Bill Review
Historically, large health plans had vast technological resources to manage payment integrity, while self-insured employers and workers compensation plans lacked the budget for giant, on-premise systems. Today, AI brings the most powerful of all programs and payment integrity capabilities to even the smallest of plans. The ability to flexibly deliver highly automated and sophisticated analysis and increased savings through a cloud-based environment means that big plans and small plans can have the most powerful FWA and overbilling detection and prevention within a matter of days.
Powered By EmbedPress