AI For Fraud Detection: A Paradigm Shift
The escalating complexity of healthcare fraud, waste, and abuse (FWA) behaviors and schemes demands a paradigm shift in how payers approach detection and prevention. Healthcare FWA losses are estimated to be at least $144B annually in the United States which represents 3–10% of total healthcare expenditures. Now, however, health plans can leverage artificial intelligence (AI) technology-based strategies to mitigate financial risks and improve both the volume and investigative efficiency of fraud detection.
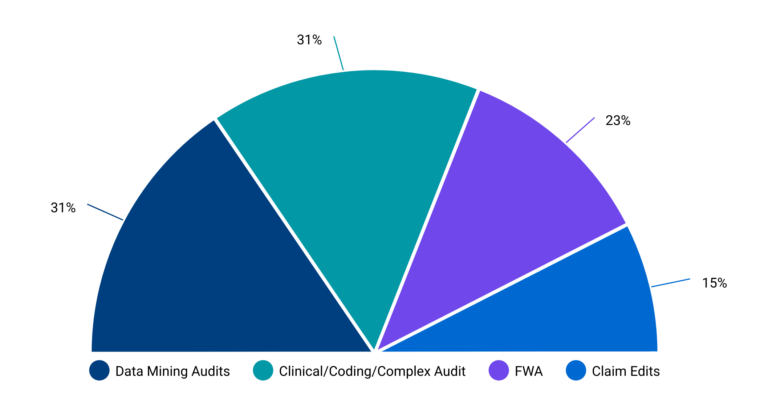
Payers recognize the potential of AI to improve FWA outcomes, with FWA being considered one of the most significant opportunities for payment integrity cost savings, alongside data mining and complex audits.
Powered By EmbedPress