In the ever-evolving landscape of healthcare payment integrity, a new approach is emerging that promises to revolutionize how we detect and prevent fraud, waste, and abuse (FWA). Our latest report, “Advanced AI in Healthcare Payment Integrity: A Provider Centric Approach,” explores how combining a provider-centric perspective with cutting-edge AI technology can transform FWA detection and prevention.
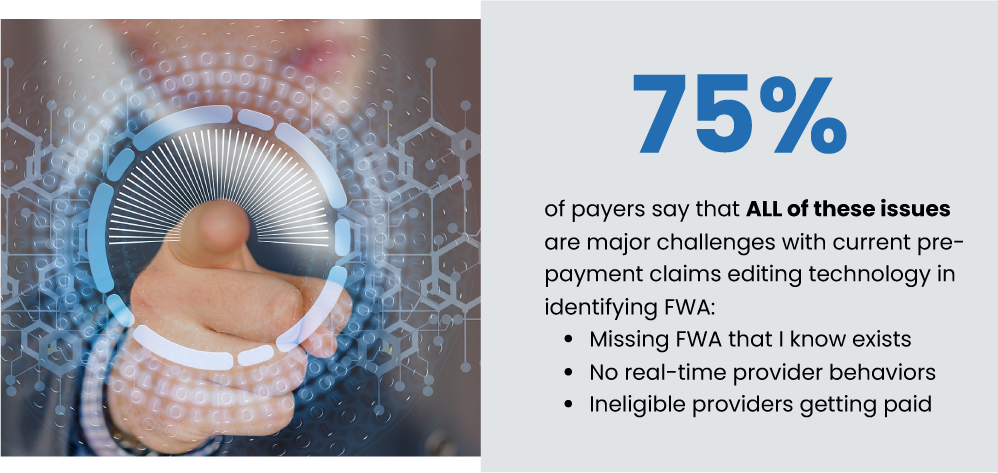
Traditional claims data-centric methods have long been the standard, but they often fall short in identifying dynamic, real-time changes in provider behaviors and relationships. Our research reveals a striking statistic:
75% of payers say that missing FWA they know exists, lack of real-time provider behavior insights, and ineligible providers getting paid are major challenges with current pre-payment claims editing technology.
This eye-opening figure underscores the urgent need for a paradigm shift in our approach to payment integrity. By adopting a provider-centric model powered by advanced AI, payers can gain unprecedented insights into provider behaviors, relationships, and patterns – potentially increasing FWA detection by 2x to 10x.
Curious to learn more about how this innovative approach could revolutionize your payment integrity efforts? Download our full report to dive deeper into:
- The limitations of legacy claims data-centric technologies
- The power of a “Know Your Provider” approach
- How advanced AI is reshaping the landscape of payment integrity
- Real-world applications of provider-centric AI in FWA prevention
Powered By EmbedPress